Here I'll point out a review paper on the "omics," the younger fields of the life sciences, including genomics, proteomics, and so forth, and their role in aging research. These fields encompass the study of biological molecules and their roles in cellular metabolism and tissue function, broken down by type and class. The study of genes, the study of proteins, the study of proteins only applicable to the immune system, the study of proteins involved in transcription, and many more divisions besides. There are now dozens of omics fields, and they continue to proliferate and specialize, this growth a reflection of the accelerating capabilities and falling costs of biotechnology. Mountains of ever more detailed data are produced each year, and merely focusing on analysis and application occupies much of the field. Indeed it might be argued that the production of omics data far outstrips its productive use at the present time, that there is something of a land grab underway now that commercial ventures focused on omics data are entering the fray, and that we are due a lengthy phase of consolidation and analysis in the years ahead. For now data is the zeitgeist of the life sciences: data on genes, on proteins, on specific clades of proteins, closely followed by the search for relevance and meaning in vast databases.
All of this is entirely in line with the goals of the scientific method: learn everything, discover everything, analyze everything. Take in all that the tools can provide. When it comes to aging, however, I think that the present zeitgeist is a distraction from an existing road to effective treatments for the causes of degeneration, frailty, and disease. It is a very effective distraction: the bulk of the field is turning in that direction, and their activities are best understood as firstly addressing the goal to comprehensively map all of our biology, and then as a distant second trying to make something of that new knowledge. Our biology is fantastically complex when operating in its standard, undamaged, youthful state. When it is disarrayed by the cell and tissue damage of aging, it can fall into a much wider range of dysfunctional operation, every older individual a special snowflake within the broader statistical patterns of disease and organ failure that we observe across populations. There is data enough here to keep the omics organizations busy for the foreseeable future, exploring the limitless differences in biochemistry found between billions of individuals as they age.
This is not the path to treating aging. It is the path to understanding exactly why there are variations in outcome when the initial types of damage that cause aging are the same for everyone. These two end goals are not the same thing at all. You cannot take the complete understanding of how aging progresses and then use it to make an effective therapy by adjusting the biochemistry of person A to make it more like the biochemistry of person B. That changes the outcome in only minor ways, at best slightly slowing the generation of damage that causes aging, or slightly improving its ongoing repair. Yet this is pretty much exactly what the mainstream of the research community is trying to do. As a goal it is enormous and challenging, and yet it will produce few benefits in the grand scheme of things.
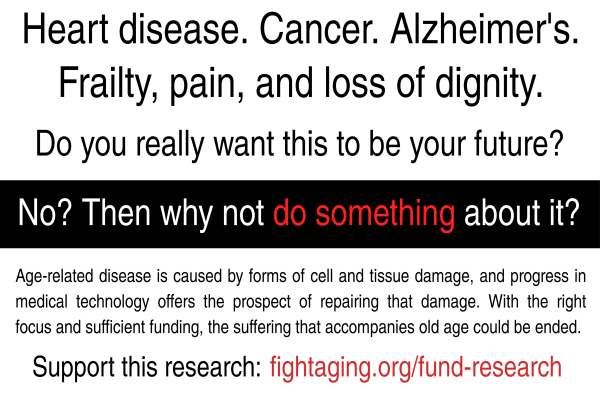
The only effective therapy for aging and age-related disease, the only way to add decades or longer to healthy, vital life spans, is to repair the damage that causes aging. We don't need omics data or much in the way of further transformative advances in the life sciences in order to accomplish that goal. The types of damage that cause aging and all of its manifestations are well cataloged and identified. The biotechnologies to repair them could be built with no major new breakthroughs, just painstaking work on the details. Yet this path of repair, to restore the undamaged youthful metabolism that we know works, is still largely overlooked.
The open access paper quoted below is an educational look at the omics fields, and illustrates just how much data there is yet to gather and analyze. The rat hole extends down for a very long way indeed. To plumb its depths will be one of the great works of this century, and I expect to be underway still decades from now. Yet even if none of that happened, the research community could still effectively cure aging and create robust and reliable rejuvenation treatments on much the same timescale, starting from where we are and what we know today about the damage that causes aging. Changing the focus of the field to fall upon periodic repair of damage is the most important thing we can help to achieve.
Integration of 'omics' data in aging research: from biomarkers to systems biology
Age is the strongest risk factor for many diseases including neurodegenerative disorders, coronary heart disease, type 2 diabetes and cancer. Due to increasing life expectancy and low birth rates, the incidence of age-related diseases is increasing in industrialized countries. Therefore, understanding the relationship between diseases and aging and facilitating healthy aging are major goals in medical research. In the last decades, the dimension of biological data has drastically increased with high-throughput technologies now measuring thousands of epigenetic, expression and metabolic variables.
Omics technologies provide valuable tools to study aging on the molecular level. Reductionist data analyses, testing the measured variables separately for association with age, have been extensively applied. Such studies successfully identified hundreds of epigenetic mutations, gene expression levels, metabolite concentrations to be linked with chronological and/or biological age (see below for details). Even though these results improved our understanding of aging as a complex phenotype, the mechanisms underlying these associations and the impact of interactions between different biological entities remain elusive in most cases. In contrast to reductionist approaches, systems biology aims to analyse all components of a biological process simultaneously taking into account their interactions and their intrinsic hierarchical structure. With more and more high-throughput data becoming available, systems biology has led to many new methods and their successful application on age and age-related phenotypes.
Genomics
Genomics was the first omics field for which high-throughput measurements became available. While aging (or rather longevity) itself was found to be only about 20% heritable, many age-related diseases are highly heritable. For instance, Alzheimer's disease (AD) shows a heritability above 70% and osteoarthritis or cataract show 50% heritability.
Epigenomics
Epigenomics describes the study of heritable changes in the genome that are not caused by DNA sequence mutations. The most common epigenetic mechanism is DNA methylation, which is known to often silence gene expression. The epigenome is influenced by environmental and lifestyle factors and is associated with many complex diseases such as neurodegenerative disorders and cancer. Nearly 500 differentially methylated regions were found to be associated with chronological age and age-related phenotypes such as lung function, cholesterol levels and maternal longevity. A recent study showed that methylation patterns of just three sites are sufficient to predict chronological age.
Transcriptomics
Genes are transcribed into RNA molecules, which are further processed in a tightly controlled process. The entirety of the RNA transcripts is referred to as the transcriptome. Similar to the epigenome, gene expression was shown to dramatically change with age. A pioneer study comparing postmortem human frontal cortex tissue samples between 30 individuals of different ages yielded 463 differentially expressed genes. Despite the small sample size, results were replicated in subsequent experiments.
Proteomics
Proteins are translated from coding transcripts. Due to alternative splicing and post-translational protein modifications, the number of proteins is estimated to be two orders of magnitudes higher than the number of genes. However, current proteomic techniques based on immunoassays, protein arrays or mass spectrometry can measure only a small fraction of the proteome. Due to these technicalities, 'proteomics' studies in aging research so far focused on smaller sets of proteins and small sample sizes. A recent study by our group analysed over 1000 proteins in 200 plasma samples. Eleven proteins were found to strongly associate with chronological age as well as age-related phenotypes such as lung function and blood pressure. The results were replicated in an independent cohort. Even though comprehensive proteomics studies are still missing, proteins are likely to be associated with several age-related diseases.
Post-translational modifications - glycomics
Post-translational modifications are important elements of proteins, which can alter their biochemical properties such as protein structure, binding preferences and enzyme activity. There are many different modifications ranging from addition of small molecules (e.g. acetylation or phosphorylation), over addition of larger molecules such as lipids or sugar chains (e.g. glycosylation), to the addition of whole proteins (e.g. ubiquitination). The application of this technology on epidemiological cohorts revealed that glycan structures are stable for one individual over time but very diverse within a population. Differences in glycomes were found to be related with various cancers. Recently, researchers showed that IgG glycans are strongly associated with age: a linear combination of three glycans explained 58% of the observed variance of chronological age in a study of four independent populations with 5117 participants in total.
Metabolomics
Metabolomics investigates the low-molecular-weight molecules in a biological system. The measured molecules are often referred to as metabolites as many of them act as educts, products and intermediates of the cellular metabolism. Currently, the Human Metabolome Database contains more than 40,000 distinct metabolites from different tissues. Similar to proteomics, to date, there is no analytical method available to determine and quantify all metabolites in a single experiment. In 2008, the first metabolome-wide association study on age analysed the plasma metabolome of 269 individuals using an untargeted approach. The authors found 100 of 300 compounds to correlate with chronological age.
Microbiomics
The human microbiome describes the complete set of microbial species (and their genomes) hosted by the human body. The largest microbial community resides in the gut, where microbial cells and their genes outnumber human cells (10:1) and genes (100:1). More than 10,000 different species with millions of protein-coding genes were identified by the Human Microbiome Project. The composition of the microbe flora varies a lot across individuals and even between different parts of the body. It has a huge influence on many biological processes such as immune response, metabolism and disease. While the microbiome seems to be relatively stable during adulthood, it changes significantly in later life. Researchers have observed drastic changes in the gut microbiome of centenarians compared with young adults as well as elderly, namely a general loss of diversity and increased abundance of bacilli and proteobacteria.
Phenomics
Simultaneously with omics data, the dimension of clinical and lifestyle traits, particularly clinically used intermediate traits, keeps increasing. Epidemiological studies collected thousands of clinically relevant phenotypes beyond omics data types. These range from anthropometric measures to health and lifestyle questionnaires. Collecting high-dimensional clinical data is important to unveil pleiotropy of genes and interactions amongst clinical phenotypes such as comorbidities. Phenomics is especially important for aging research. Dozens of clinical phenotypes, such as Parkinson's, AD, body mass index, blood pressure and bone mineral density, as well as lifestyle parameters, such as nutrition, smoking and physical activity, are strongly related to age. Only extensive collection of data and their joint analysis will help to unveil these dependencies and find causal relationships.