A Look Back at the Science of Longevity and Advocacy for Rejuvenation in 2017
Another year is over, and we're all that much closer to both the ugly declines of aging and the advent of rejuvenation therapies. For those fortunate enough to be in a younger demographic, which of those two items wins out depends entirely on the pace of progress. We are in a race. The results matter greatly. Every effort made to help will shift the odds to be that much better.
A Year of Ups and Downs in Fundraising
Insofar as fundraising goes, this has been a mixed, interesting year of ups and downs. On the one hand it has been a struggle to raise funding for smaller non-profit projects, such as the MouseAge and AgeMeter initiatives at Lifespan.io. At the same time companies working on rejuvenation biotechnology have obtained angel and venture investments, and new venture funds are entering the longevity science community. Ichor Therapeutics announced a series A for their SENS-based Lysoclear technology, and later in the year their other spin-off Antoxerene was funded. Oisin Biotechnologies expanded their technology to target cancerous as well as senescent cells, and are also raising more funding. Other companies involved in senescent cell clearance have done well; SIWA Therapeutics pulled in new funding for their antibody approach, for example, and CellAge was seed funded to work on better assays for senescence. Unity Biotechnology continues to have enough of a war chest to buy the rest of the nascent industry should they so choose. AgeX Therapeutics launched, with Aubrey de Grey on their staff - that should be interesting. LIfT Biosciences seems to be doing well in their efforts to bring leukocyte transfer therapies for cancer to the clinic.
On the other side of the fundraising fence, the Methuselah Fund launched this year, taking a mixed non-profit/for-profit approach, and from the funds raised from our community invested in Leucadia Therapeutics, supporting a new approach to clearing aggregates that cause neurodegeneration. Larger monied interests arrived in the form of Jim Mellon's Juvenescence venture, who have initially invested in Insilico Medicine, but have indicated support for the SENS research agenda. As this is a vocal group, we can expect to see them influencing public and investor opinion rejuvenation research and development in the years ahead.
Despite all of the challenges faced by non-profit fundraisers over the course of much of 2017, the year ended on a high point: the SENS Research Foundation year end fundraiser pulled in $1 million more than the target of $325,000 or so in pledges, as the anonymous principal of the Pineapple Fund donated $1 million in bitcoins in December. The Fight Aging! SENS Patron component of that year-end fundraiser came to a successful conclusion: Josh Triplett, Christophe and Dominique Cornuejols, and Fight Aging! put up a $36,000 challenge fund to match the next year of monthly donations, and that target was reached. Many thanks are due to all who supported SENS rejuvenation research over the course of the year: this funding makes a real difference, especially now that multiple lines of research are closing on the point at which commercial development can begin. You might take a look at the SENS Research Foundation annual reports and the state of progress in SENS addition to the Fight Aging! FAQ for a sense of how things are going.
Finally, with all of the hype surrounding blockchain initiatives this past year, it was inevitable that some of the adventurous souls in our community would make the effort to run initial coin offerings and see whether or not this was a viable path to pull in funding. The Open Longevity organization set out to give it a try, and so did Youthereum. It is a little early to say where this will all go; it is a very rapidly changing area of effort.
Expanding Efforts in Advocacy
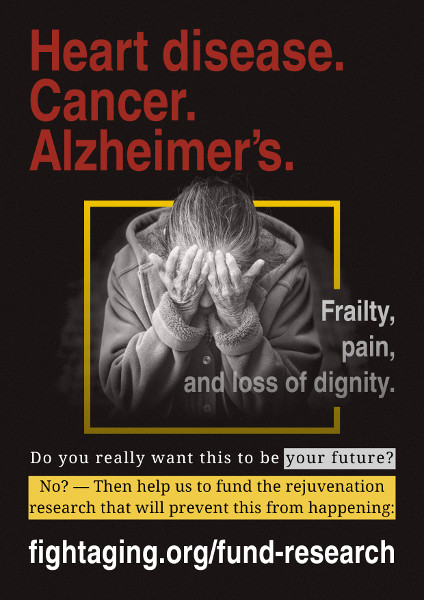
Discussion of advocacy for the cause is a usual feature of our community, as we try things and attempt to make progress in persuading the world that rejuvenation research is plausible, practical, and necessary. There are more people engaged in advocacy now than at any time in the past decade, and so discussions of strategy come up often. New ventures kicked off in 2017 include the Geroscience online magazine, and among the existing ventures the LEAF / Lifespan.io volunteers seem to be hitting their stride. The mainstream media continues to be as much a hindrance as a help, and where it is a help you will usually find Aubrey de Grey involved in the article somewhere - which is not to mention the recent /r/futurology AMA.
In the broader question of strategy in advocacy, questions abound. Do we continue to spend a lot of time tearing down arguments against treating aging as a medical condition, such as the naturalistic fallacy and unfounded fears of overpopulation? Should we be avoiding talk of immortality and radical life extension? Or focusing on ethical arguments? Or correcting mistaken views of aging and the underlying biology? Trying harder to persuade people that rejuvenation therapies are a near future possibility? Or trying to address some of the unhelpful behavior from some members of the research community? Or continuing to hammer on the costs of failing to address aging, the worldwide toll of death and suffering? Or continue to hammer on the benefits of success? Do we talk less and strive to engage with structural problems in the funding of research? Or endeavor to find more funding for advocacy rather than sending it all to research? Given the fact that we have to keep making the same arguments for incremental gains, are we bad at this advocacy business, or is it a tough challenge? Should we switch some of this non-profit activity to for-profit activity?
We must keep making the case, of course - the benefits of success are enormous. There were some sizable wins in advocacy this year, such as a series of YouTube videos from popular channels that covered the prospects for the treatment of aging and were viewed by hundreds of thousands of people.
Topics in Longevity Science from the Past Year
Is genetics important in longevity? Some researchers think that most of the observed variation in human life span is chance, not genes. There has been plenty of other research this year on human genetics that are related to longevity, and there are a number of large commercial ventures working in the space, but it is going to be hard to top the discovery of human PAI-1 mutants who appear to enjoy a seven year gain in life expectancy. Since this mutation is closely connected to cellular senescence, it seems plausible that we should read this as support for the benefits of senolytic therapies. A similar discovery was made for a growth hormone variant, with a much smaller effect, of course. That aside, analysis of genetics doesn't look like a fast road to sizable results for a variety of good reasons.
Cellular senescence research continues apace, of course, alongside the commercial efforts to bring senolytic therapies to the clinic. The research community has now well and truly woken up on this topic, and many researchers are increasingly optimistic that senolytic treatments will be transformative for medicine. New work now implicates cellular senescence in kidney disease, macular degeneration, osteoarthritis, cardiac hypertrophy, sarcopenia, lung diseases, vascular calcification, immune system aging, fibrotic diseases, fatty liver disease, skin aging, declining regenerative capacity, the accelerated aging effect of chemotherapy, the effects of visceral fat on health, and more.
Some groups are trying to find ways to reverse senescence, sabotage harmful signaling by senescent cells, or prevent cells from entering this state - though it is unclear as to whether or not these classes of approach will be significantly helpful, given that the cells are damaged. The more direct and definitively effective approach of destroying senescent cells continues to gather more potential methods. This past year, the very intriguing method involving FOXO4-DRI was demonstrated in mice - we can hope it holds up in human studies, as this looks considerably better than the current crop of repurposed chemotherapeutic senolytic pharmaceuticals. Those chemotherapeutics expanded to include HSP90 inhibitors quite recently. Meanwhile exploration continues in search of better ways to assess the number of senescent cells in tissues; current approaches just aren't all that useful for human clinical applications.
Beyond clearance of senescent cells, other lines of SENS research are progressing. This year, glucospane research turned to the creation of monoclonal antibodies to aid in building a therapy to break cross-links in aged tissues. Gensight continues to find success in their implementation of allotopic expression of mitochondrial genes, proving out the technology platform that will ultimately become a rejuvenation therapy.
Given the advanced state of senolytics, it is only natural that our community is starting to think about trials and how to run them - in addition to whatever the various companies in the space might put together over the next couple of years. Paid trials are a good idea, but there is an unaccountable amount of hostility towards them from the scientific community. Groups such as Betterhumans and the Society for the Rescue of Our Elders are running small, independent senolytic pilot studies. Responsible self-experimentation is another time-honored way forward. Some people are trying it for senolytic treatments. I have put some thought into the logistics and what tests one might use in order to determine whether or not a particular treatment is useful.
Self-experimentation in the broader community nowadays extends to comparatively crude gene therapies, with a number of organizations offering the tools or running the trials. These technologies are too cheap and too easily used to be more than inconvenienced by regulators. A few companies are headed in the same direction, such as Libella Gene Therapeutics, with a plan for human telomerase gene therapy trials, following in BioViva's footsteps.
Lines of research emerging from parabiosis studies, in which old and young individuals have their circulatory systems linked, continue to expand. The core questions regarding whether beneficial factors in young blood or harmful factors in old blood are responsible for the observed effects on aging, or both and to what degree, continue to be debated. While the weight of evidence leans towards "bad old blood" with a few specific candiates for the factors causing that effect, it is still the case that new studies with evidence for beneficial factors in young blood continue to arrive. The contradictions will eventually be resolved, but for now it is an area of research in flux. Meanwhile, human trials of plasma transfusion from young to old continue; Ambrosia and Alkahest reported results that are ambiguous enough to resolve nothing.
Cryonics remains an important and underappreciated technology. Not all of us are going to make it; the progression of rejuvenation technology won't happen fast enough. We will need the backup plan of cryonics. This year marks the fiftieth anniversary of the first, comparatively crude cryopreservation, and that individual, unlike most of those from of that era, remains preserved. The technologies of preservation today are far more advanced, and the organizations more reliable in the face of various failure modes, as noted in an interview from earlier in the year. One line of work that has made considerable progress of late is safe and rapid thawing of vitrified tissues. In community news, the International Longevity and Cryopreservation Summit took place in Spain earlier this year.
Is Google's large investment in aging research, the California Life Company, Calico, at all relevant to the goal of defeating aging? The more we find out, the less likely it appears. Researchers are increasingly willing to go on record as saying that the efforts funded there are just not helpful in the near term. Calico looks like pure curiosity-driven scientific research into understanding the very fine details of aging, which is not what we need at this stage in order to push forward to the range of effective therapies that can be built in the near future.
Amyloid accumulation is one of the causes of aging, and transthyretin amyloid is one of the types of amyloid with more research interest. It is connected to heart disease and osteoarthritis, and may be the majority cause of death in supercentenarians. Covalent Bioscience is one of the companies looking at ways to remove this amyloid. A variety of new research was published this past year, including a better approach to assessing the amount of amyloid present, and RNA inteference and antibody based therapies.
On the topic of biomarkers of aging, there are many various lines of work taking shape. The research community agrees that having effective, reliable biomarkers for a rapid assessment of biological age is very necessary to speed up progress towards treatments for aging. Among efforts noted this year include gene expression of glia, metrics based on neuroimaging, or on microRNA expression, various attempts to assemble a compound biomarker from a collection of standard lab tests and measures. People are setting up online databases to hold the various prospects. DNA methylation tests based on one or more of the existing epigenetic clocks have now reached the consumer marketplace. They can be ordered from Osiris Green and Zymo Research. The research community continues to refine and expand further epigenetic clocks and related assessments.
Calorie restriction is ever a popular research topic, despite this being unlikely to produce very large effects on human lifespan. This is really the core of the geroscience view of the treatment of aging: slow it down a bit, but don't try for more. Researchers now claim that human studies show a slowing of aging via a collection of biomarkers. The final consensus on long-running primate studies appears to be that, yes, calorie restriction does modestly slow aging in our near relatives. Near all specific measures of aging are similarly slowed, such as the fibrosis leading to kidney disease, the early stages of cancer, the epigenetic changes of aging, the decline of the immune system, the accumulation of metabolic waste in cells, and the accumulation of amyloid in aged tissues. Researchers continue to find new mechanisms by which calorie restriction produces its effects, such as a slowing of ribosomal activity. Sense of smell continues to surprise the research community in the degree to which it is important in determining response to calorie intake. A number of researchers have gained traction in pushing forward intermittent fasting as an alternative approach, particularly the fasting mimicking diet. Meanwhile, ever more candidate drugs and protein targets are found that might act as a basis for potential calorie restriction mimetic therapies - though given the lack of concrete progress on this front over the past decade, I wouldn't hold my breath waiting for results.
Another rising topic in aging research is the contribution of gut microbes and other microbial populations in the body; these may be as influential over aging as, say, exercise or calorie intake. Researchers have noted influences on amyloid accumulation, something that is attracing greater interest from the Alzheimer's research community. It is also interesting to see studies demonstrating extended life as a result of transplantion of gut bacteria from young animals to old animals in zebrafish and in mice, or showing that healthier older individuals have microbial populations more like those of younger individuals. Moving beyond observations, candidate mechanisms are being discovered to explain exactly why changes in gut bacteria are good or bad. The next step is therapies that target those mechanisms. Researchers appear close to being able to sabotage the detrimental effects of oral bacteria, for example.
A few interesting views on aging and its origins surfaced in the past year: aging as a consequence of complexity in cellular life, for example, or that aging is an inevitable consequence of competition between cell types in multicellular life. Another group argued for selection to decline with age even in hypothetical immortals, thus ensuring that no species would become so exceptionally long lived. Others have looked for explanations for the present state of stem cell populations, in that they are not as effective as they could be, especially in later life.
Work on addressing dysfunction in the immune system by destroying near all immune cells and then repopulating them via cell therapy, shown to cure severe autoimmune disease is progressing on a number of fronts. The most important thing here is to find a safer, less damaging way to kill the unwanted parts of the immune system. Currently it is too risky to be applied to older people, so as to clear out the issues in an aged immune system. Researchers recently discovered a promising lead here.
Regenerative medicine, cell therapies, and tissue engineering are energetic fields. Far too much is going on to note all of it, but a few things caught my eye. The Methuselah Foundation continues to be in the thick of it with their initiatives to promote progress, for example. Decellularization continues to be an important line of research, and that will be the case until someone figures out a reliable means of producing blood vessel networks. Bioprinting of tissue proceeds apace, and is driving a lot of the advances in reduced cost and increased capabilities. Researchers are building ever more and better organoids: fully functional ovaries, stomach, skin that is fully and completely structured, lungs, thymus, bile ducts, inner ear, and more. Organoid production is on the verge of scaling up, and use of multiple organoids may work well as an alternative to full organ transplant for some organs. In other parts of the tissue engineering field, mass production is also an ongoing interest. Organ factories are not so very far ahead. Teeth are similarly moving forward; tooth regrowth has moved up from rodents to canines. Researchers are also making inroads into the manufacture of blood to order.
Will regenerative medicine make the leap soon from cell therapies that do little but suppress inflammation, to actual methods of rejuvenation and repair? That is hard to say, and the final form of such therapies is also uncertain. Consider induced cell turnover or artificially increased cell replication strategies for example, a novel approach where the implications have yet to be fully explored, or the variety of cell therapies that appear to produce quite sizable changes despite using only incremental advances in methodology, or very novel processes such as reprogramming skin cells into stem cells in a living individual. Comparative biology continues to deliver intriguing findings from lizards, spiny mice, zebrafish, and the like. Related work is finding that adjusting the balance between populations of macrophages with different polarizations can spur greater regeneration in mammals, and the same may be true of microglia.
2017 Short Essays
You'll find a number of short essays at Fight Aging! each year. Here is a selection from 2017:
- Why Rejuvenation Research Startups Go Quiet Following Launch
- Will Senescent Cell Clearance Therapies Sink the Pensions and Annuities Industry?
- The Million Year Life Span
- If Much Older than 30, Save More Aggressively Over the Next Decade or Two
- What Next for Unity Biotechnology?
- The Problem with Focusing on Healthspan
- Advocacy for Rejuvenation Research is as Much a Process of Documentation as it is a Process of Persuasion
- The Fall into Nihilism
- Success in Rejuvenation Research to Date is Partial: Many Projects Still Need Our Philanthropic Support to Flourish
- Wolf has been Cried So Very Many Times When it Comes to Anti-Aging Therapies
- Patient Paid Clinical Studies are a Good Plan for Rejuvenation Therapies
Looking Ahead to 2018
Next year should see the first published results from senolytic trials - and if the effects of the first drug candidates translate well from mice to humans, that should wake up everyone not yet aware of the enormous potential of this field. I expect that this will probably overshadow everything else achieved in the field for a while, at least in the public eye. There will be more startup companies launched to work on SENS rejuvenation biotechnologies, and that will hopefully be an ongoing story for the next few years. This period of transition, handing off from laboratory to clinical development, is critical to the future of human rejuvenation therapies. The more we can do to help, the better.